CSID Genetics Overview
Congenital Sucrase-Isomaltase Deficiency (CSID) is a rare carbohydrate malabsorption disorder that produces chronic diarrhea, abdominal pain, gas, distention, and bloating in patients who have a sucrase-isomaltase enzyme deficiency. The sucrase-isomaltase enzyme is necessary for digesting dietary sucrose and starch for absorption in the small intestine.
CSID is an autosomal recessive condition requiring both copies of the sucrase-isomaltase (SI) gene to be pathogenic variants, resulting in diminished sucrase-isomaltase activity and clinical symptoms. There are 37 identified single pathogenic nucleotide polymorphisms (SNPs), nonsense mutations (inserted stop codon) and deletions in the SI gene described in the literature that have been associated with CSID.1-9 Single nucleotide polymorphisms result in single amino acid changes in the sucrase-isomaltase glycoprotein, which manifests with a variety of biochemical phenotypes, ranging from phenotypes manifesting as a lack of enzyme activity due to various enzyme transport defects, to improper folding of the enzyme protein 3D structure.6 In addition, there are seven described phenotypic expressions of SI pathogenic variants, and a spectrum of CSID symptom severity.6
An SI gene mutation may, but does not always, lead to a reduction of SI expression or function. Therefore, the manifestation of clinical phenotypes and symptom severity varies.1 The contributing factors are not well known and are possibly related to environmental factors such as overall intestinal health, gastrointestinal infections and diet, especially the amount of sugar and starch consumed.
The SI gene is located on the long arm (q) of chromosome 3 at position 26.1.10
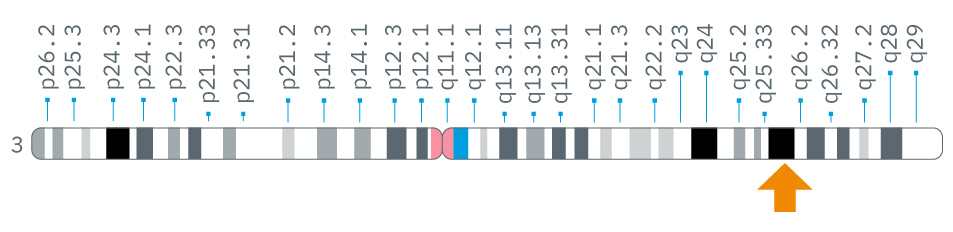
Credit: Genome Decoration Page/NCBI
Figure 1: Location of the SI gene on chromosome 3 at position 26.1.10
Practice Tip
If a pediatric patient is diagnosed with CSID, related symptomatic family members may also benefit from diagnostic tests for possible CSID.
Practice Tip
Genetic testing for pathogenic SI variants is available, but the genetic test only screens for known variants. If a patient has one or more variants that have not yet been investigated for potential pathogenicity, these will not be identified in a genetic test. Thus, there is a risk that a genetic test for CSID may result in a false negative.
- Uhrich S, Wu Z, Huang JY, Scott CR. Four mutations in the SI gene are responsible for the majority of clinical symptoms of CSID. J Pediatr Gastroenterol Nutr. 2012;55(suppl 2):S34-S35. doi:10.1097/01.mpg.0000421408.65257.b5
- Alfalah M, Keiser M, Leeb T, et al. Compound heterozygous mutations affect protein folding and function in patients with congenital sucrase-isomaltase deficiency. Gastroenterology. 2009;136(3):883-92. doi:10.1053/j.gastro.2008.11.038
- Gericke B, Amiri M, Naim HY. The multiple roles of sucrase-isomaltase in the intestinal physiology. Mol Cell Pediatr. 2016;3(1):2-6. doi:10.1186/s40348-016-0033-y
- Jacob R, Zimmer KP, Schmitz J, et al. Congenital sucrase-isomaltase deficiency arising from cleavage and secretion of a mutant form of the enzyme. J Clin Invest. 2000;106(2):281-7. doi:10.1172/JCI9677
- Keiser M, Alfalah M, Pröpsting MJ, et al. Altered folding, turnover, and polarized sorting act in concert to define a novel pathomechanism of congenital sucrase-isomaltase deficiency. J Biol Chem. 2006;281(20):14393-9. doi:10.1074/jbc.M513631200
- Naim HY, Heine M, Zimmer KP. Congenital sucrase-isomaltase deficiency: heterogeneity of inheritance, trafficking, and function of an intestinal enzyme complex. J Pediatr Gastroenterol Nutr. 2012;55(suppl 2):S13-20. doi:10.1097/01.mpg.0000421402.57633.4b
- Ritz V, Alfalah M, Zimmer KP, et al. Congenital sucrase-isomaltase deficiency because of an accumulation of the mutant enzyme in the endoplasmic reticulum. Gastroenterology. 2003;125(6):1678-85. doi:10.1053/j.gastro.2003.09.022
- Sander P, Alfalah M, Keiser M, et al. Novel mutations in the human sucrase-isomaltase gene (SI) that cause congenital carbohydrate malabsorption. Human Mutat. 2006;27(1):119. doi:10.1002/humu.9392
- Spodsberg N, Jacob R, Alfalah M, et al. Molecular basis of aberrant apical protein transport in an intestinal enzyme disorder. J Biol Chem. 2001;276(26):23506-10. doi:10.1074/jbc.C100219200
- SI sucrase-isomaltase [ Homo sapiens (human) ]. National Library of Medicine (US), National Center for Biotechnology Information. Last updated April 7, 2025. https://www.ncbi.nlm.nih.gov/gene/6476