CSID Symptoms
For patients with Congenital Sucrase-Isomaltase Deficiency (CSID), living with postprandial symptoms such as chronic diarrhea, abdominal pain, distention, gas, and bloating is difficult and can limit quality of life.
Consider these patient cases:
- Jeremy is a 7-month-old boy with chronic, explosive diarrhea, and bowel movements 5 to 19 times per day. He has been losing weight, shows signs of dehydration, and has excoriated buttocks. His mom has been weaning him from breast milk and introducing some solid foods and juices.
- Matilda, a 35-year-old woman, has a body mass index (BMI) of 16.5 kg/m2 and says she has suffered intermittent diarrhea, abdominal pain, and bloating after eating ever since she was a child. Her abdomen is flat in the morning upon waking, but becomes increasingly distended throughout the day.
While their ages are very different, both patients exhibit the typical symptoms associated with a carbohydrate malabsorption, which could be caused by CSID. These symptoms merit further investigation to reach the right diagnosis and select the best treatment approach.
CSID Symptoms
In patients with CSID, reduced or absent sucrase-isomaltase enzyme activity results in the presence of undigested dietary sugars and starches in the lumen of the small intestine and the colon, which accelerates the transit time of the entire meal through the small intestine. Colonic microflora then ferment the unabsorbed substrates. Sucrose is the most clinically significant substrate because it results in rapid fermentation, which releases methane, hydrogen, and carbon dioxide gases and causes abdominal pain, flatulence, bloating, and abdominal distention.
Sucrose Digestion: Normal Digestion and Symptoms With CSID
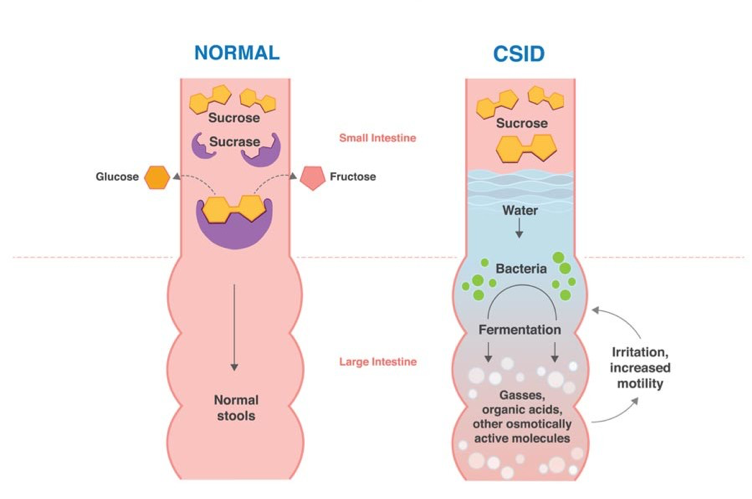
Figure 1. Normally, dietary sucrose (yellow) is digested by sucrase into two subunits, glucose (gold) and fructose (pink), which are rapidly absorbed into the bloodstream, resulting in normal stools. With CSID, sucrase is absent or dysfunctional and dietary sucrose is not digested into its two subunits. Thus, sucrose is not absorbed by the small intestine and undergoes bacterial fermentation in the large intestine. The fermentation byproducts are gases, organic acids, or other osmotically-active molecules, causing postprandial abdominal distention and pain, and water retention producing watery, acidic diarrhea. Symptom severity can vary, depending on the amount of sucrose and starch ingested and the degree of sucrase and/or isomaltase enzyme activity present.
The presence of undigested food in the colon, especially carbohydrates, can alter the osmotic gradient, resulting in watery diarrhea. Frequent diarrhea can result in a positive feedback loop causing accelerated small-bowel transit. A rapid small-bowel transit decreases the time for enzymatic digestion and subsequent absorption, which leads to increased fermentation, which, in turn, leads to more diarrhea and rapid small-bowel transit, which can result in malabsorption of all nutrients.1-3
Overall, the reduced absorption of essential nutrients can lead to malnutrition and failure to thrive in children, or low body weight in adults. Moreover, accelerated bowel transit can hinder the absorption of other nutrients such as fat and monosaccharides, as well as impair the function of normal, postprandial hormones that regulate gastrointestinal processes such as insulin, gastric inhibitory peptide, peptide YY, GLP-1, and C-peptide.3,4
Chronic symptoms of CSID may include:
- acidic, watery diarrhea
- abdominal pain, cramps
- abdominal distension
- flatulence
- excoriated buttocks, diaper rash
- nausea and vomiting
- dyspepsia
- failure to thrive
- weight loss
Symptoms in infants with CSID usually manifest when they are weaned from breast milk and start to ingest foods containing sucrose and starches, such as juices, teething biscuits, baby-food fruits, and medications sweetened with sucrose. Symptoms are usually more severe in children than in adults because they have shorter small intestines and a reduced reserve capacity in the colon to absorb excess luminal fluid.1,2
Although symptoms persist in adults, they may be less severe than those observed in children. Adults may note an increase in bowel movement frequency with loose stool formed, and experience diarrhea only after ingesting food containing high levels of sucrose. They may also alternate between diarrhea and constipation, depending on their diet and use of anti-diarrheal medications, which might mask classical CSID symptoms, thus leading to a misdiagnosis of mixed-type or diarrhea predominant irritable bowel syndrome (IBS).
While most individuals affected by CSID present with classic symptoms, many are given a nonspecific diagnosis of toddler’s diarrhea as infants and young children. Many patients who achieve normal growth are not diagnosed with CSID until they are between the ages of 2 to 8 years, or even later in adolescence or adulthood. A careful evaluation of symptoms will inform the next steps for diagnosing carbohydrate-malabsorption attributed to an enzyme deficiency such as CSID.
- Treem WR. Clinical aspects and treatment of congenital sucrase-isomaltase deficiency. J Pediatr Gastroenterol Nutr. 2012;55(suppl 2):S7-S13. doi:10.1097/01.mpg.0000421401.57633.9
- Cohen SA. The clinical consequences of sucrase-isomaltase deficiency. Mol Cell Pediatr. 2016;3(1):5. doi:10.1186/s40348-015-0028-0
- Gericke B, Amiri M, Naim HY. The multiple roles of sucrase-isomaltase in the intestinal physiology. Mol Cell Pediatr. 2016;3(1):2-6. doi:10.1186/s40348-016-0033-y
- Treem WR. Congenital sucrase-isomaltase deficiency. J Pediatr Gastroenterol Nutr. 1995;21(1):1-14. doi:10.1097/00005176-199507000-00001